How might we help patients complete the bladder cancer diagnosis process?

Background
Each year, roughly 1,500 patients at University of Pennsylvannia Hospital System (UPHS) find out they have Microscopic Hematuria, a condition where small, non-visible amounts of blood show up in their urine. When these findings come in, patients are advised to see a Urologist to get tested for bladder cancer. Out of all those patients, 200 fail to finish the process. Given current statistics, it’s likely 20 of those 200 have bladder cancer. Our team set out to answer the question—is there a way to help more patients to complete this process?
A typical journey
 *Name changed to protect identity
*Name changed to protect identityTake for example Steven. For the past 5 years Steven’s doctor has been telling him he should see a Urologist about blood in his urine. When our team chatted with him on the phone, we learned this wasn’t Steven’s only health concern. Steven had a heart attack a few years ago and has been doing his best to eat better. When asked about his urology appointment, he said, “I don’t even remember why I missed that...”
Steven’s attitude towards urology is common. Of the 27 patients we spoke to who had recently missed their New Patient Visit (NPV) appointment, the lack of urgency was pervasive.
Insights
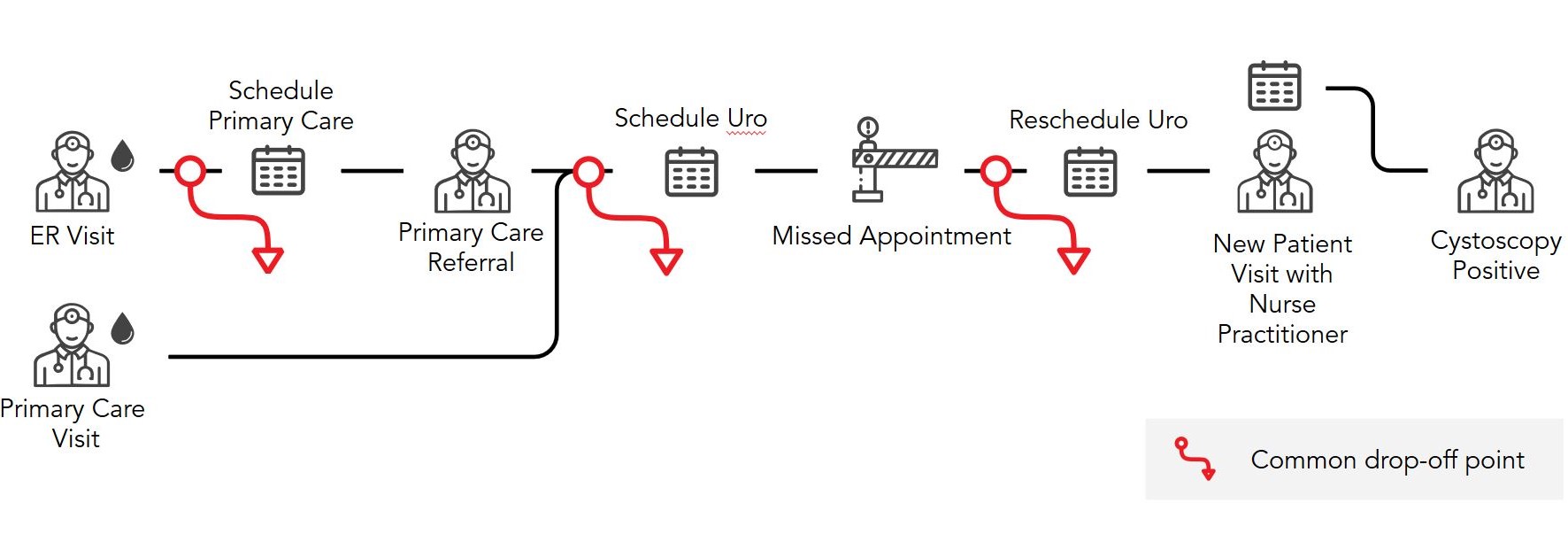
Throughout our research, we honed in on two key factors that drove this lack of urgency. First, many of the patients have microhematuria, a condition that is painless and invisible to the naked eye. When there are no symptoms the issue seems unimportant. Second, as shown in the journey above, there are many steps in the diagnostic process. The multitude of steps and long scheduling timelines communicate to the patient a lack of urgency.
Testing our first hypothesis
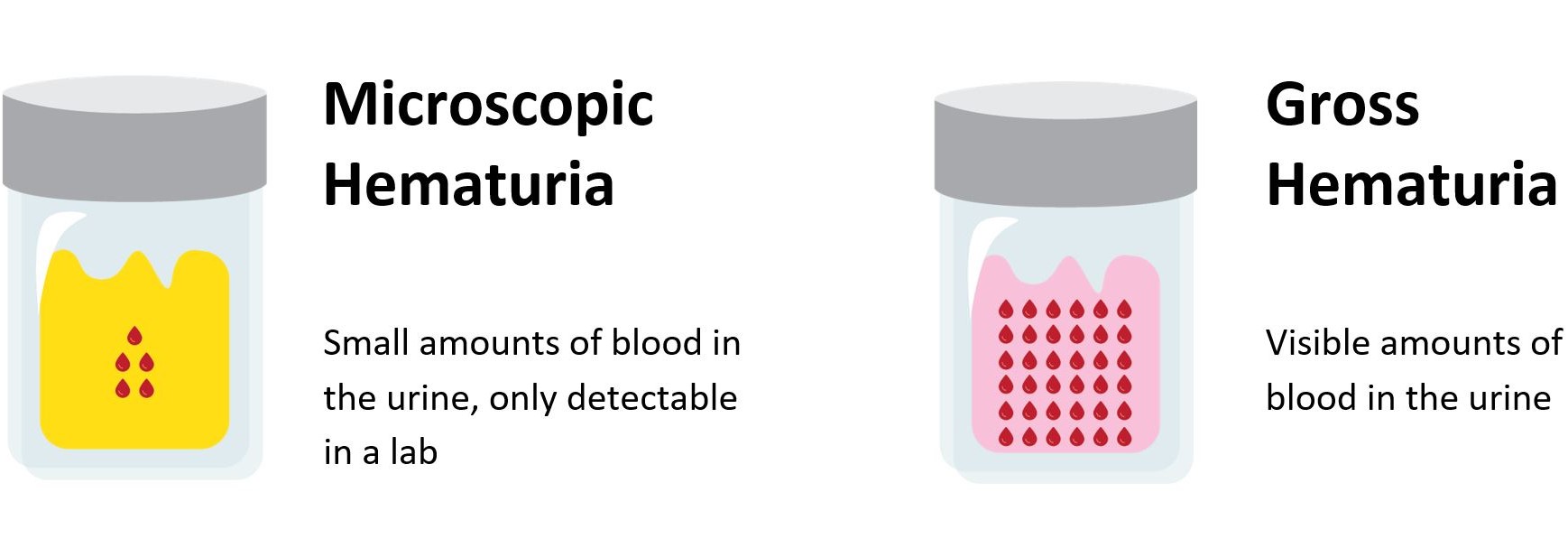
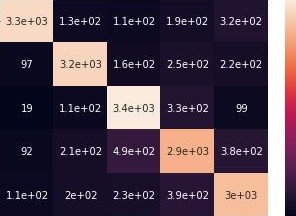
Our first hypothesis was that if we sent all new microhematoria patients a nudge and explanation of symptoms, then they'd be more likely to come in. With the help of the Center for Healthcare Innovation, we send all new microhematuria patients a mailer with above graphic, statistics on bladder cancer, and an appointment reminder. We tested this pilot for 60 days and saw a minor uptick in completions rates.
Changing course
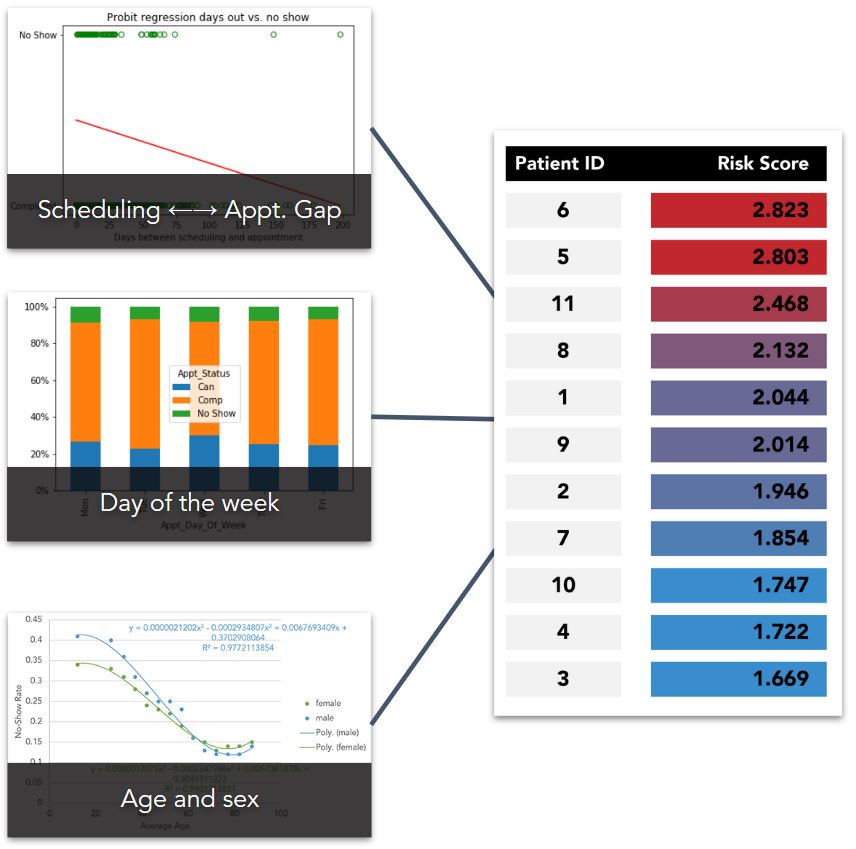
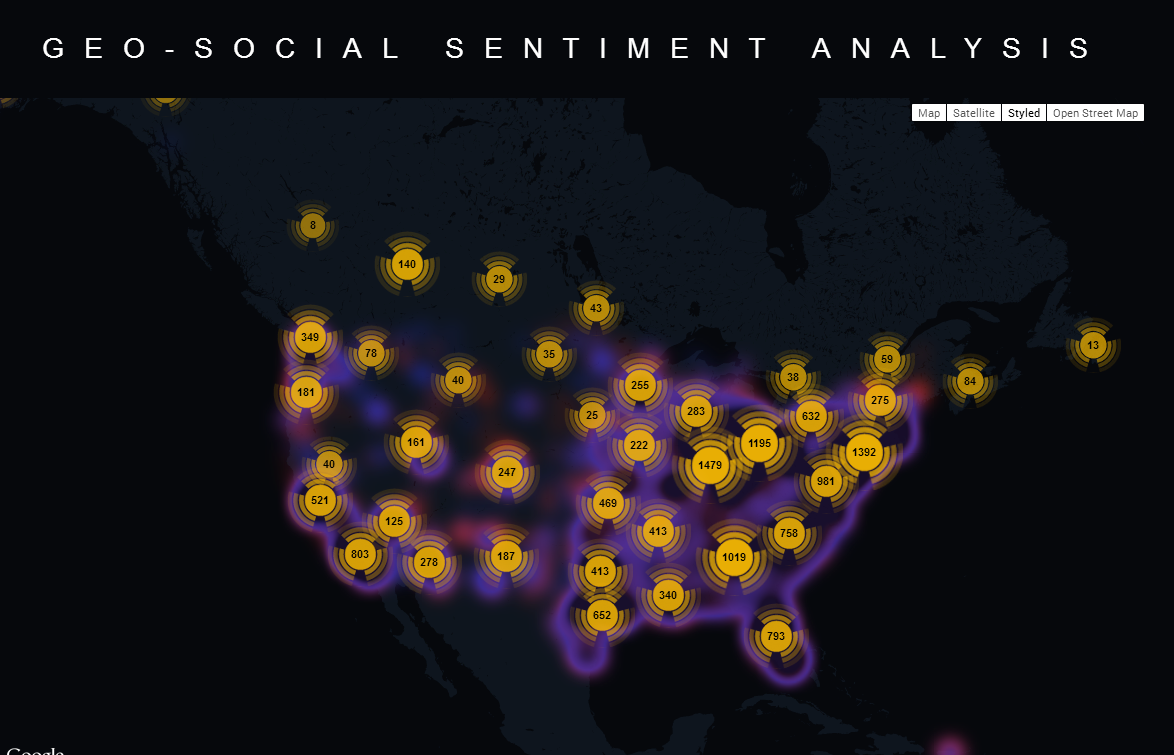
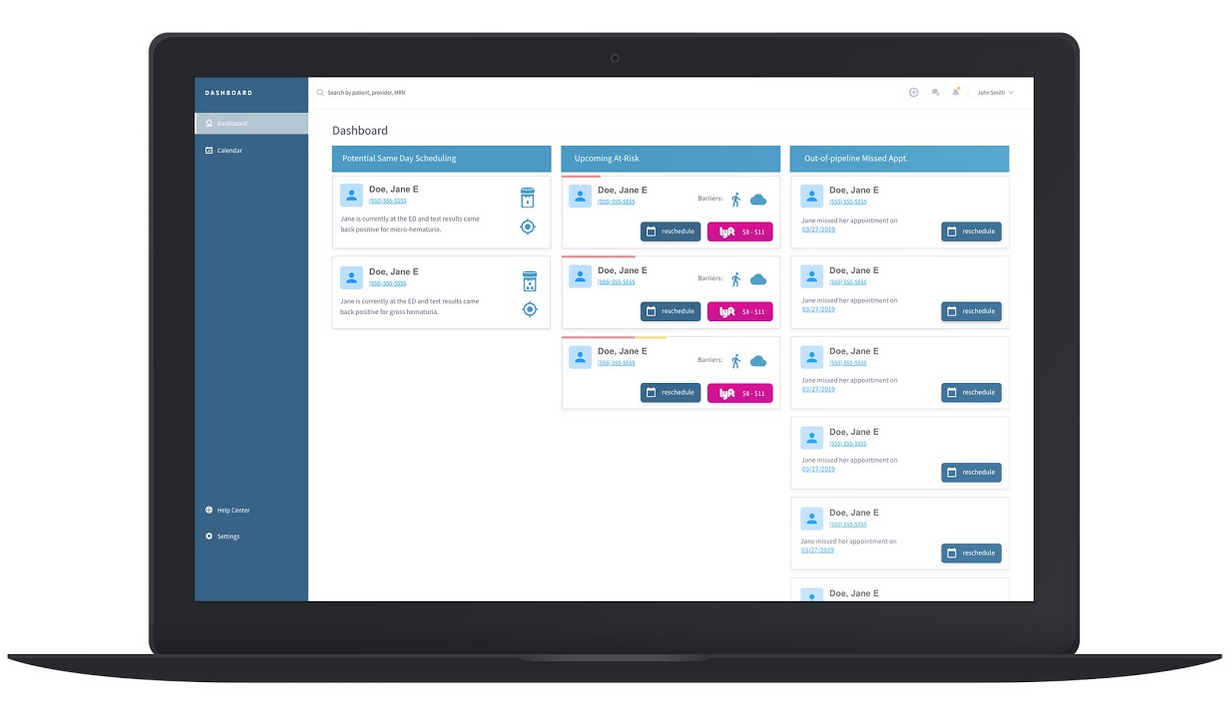
After chatting with patients and looking at the data we realized the mailers helped but not as much as we had hoped. Many patients still missed their appointment because the mailer got tossed in the garbage or because something came up last minute. With these new insights in mind, we decided to shift tactics. Our new hypothesis was that if we called high no-show risk patients the day before their appointment, we would be more likely to get them to their appointments. Using series of clickable prototypes, we ran mock simulations with the staff to test how quickly they could identify and call 3 high-risk patients. With those observations in hand, we developed the interface shown below. Unfortunately, there was not enough time to run a large scale test to see if this high touch intervention worked across the population, but in our short tests we saw fantastic positive response.
Conclusion
Getting everyone to show up to their appointments is a difficult task. (And it is often more a factor of the complexity of healthcare processes than the determination of a patient.) While there's still a lot to be done to shorten the diagnostic process, I'm glad we were able to give the urology team a few tools and ideas for the future.